Histamine Intolerance Symptoms: 47 Symptoms to ...
Histamine intolerance is becoming increasingly identified as an underlying cause of numerous strange, allergy-like symptoms, which often appear without any history of such issues.And, as histamine intolerance symptoms can be body-wide,...
Histamine Intolerance Symptoms: 47 Symptoms to ...
Histamine intolerance is becoming increasingly identified as an underlying cause of numerous strange, allergy-like symptoms, which often appear without any history of such issues.And, as histamine intolerance symptoms can be body-wide,...

Histamine Allergies: Symptoms, Causes, and Trea...
The symptoms, causes, and treatments of histamine allergies can be confusing if you're unsure where to begin. Having personally dealt with histamine intolerance, I understand how challenging it can be...
Histamine Allergies: Symptoms, Causes, and Trea...
The symptoms, causes, and treatments of histamine allergies can be confusing if you're unsure where to begin. Having personally dealt with histamine intolerance, I understand how challenging it can be...

Low Histamine Recipe: Breakfast Apple Pie (Suga...
I was planning on waiting to post this, but I kept on getting inbox messages and honestly am so excited about it that I had to drop everything to bring...
Low Histamine Recipe: Breakfast Apple Pie (Suga...
I was planning on waiting to post this, but I kept on getting inbox messages and honestly am so excited about it that I had to drop everything to bring...

Low Histamine Chicken Salad Buddha Bowl Recipe
Buddha bowls are in!...and there's so much to love about them. They're a great way to pack small portions of a variety of nutritious foods into one dish. They're fresh,...
Low Histamine Chicken Salad Buddha Bowl Recipe
Buddha bowls are in!...and there's so much to love about them. They're a great way to pack small portions of a variety of nutritious foods into one dish. They're fresh,...
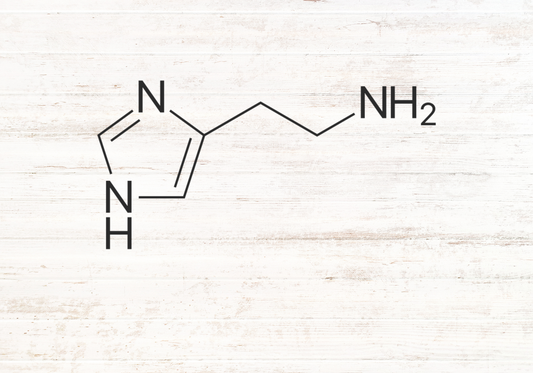
What is Histamine Intolerance? The Ultimate Guide
If you've been itching and scratching in response to food, developing hives and anxiety and even digestive issues to boot, there's a chance you may have histamine intolerance.What’s histamine intolerance,...
What is Histamine Intolerance? The Ultimate Guide
If you've been itching and scratching in response to food, developing hives and anxiety and even digestive issues to boot, there's a chance you may have histamine intolerance.What’s histamine intolerance,...

Low Histamine Broccoli Bread Recipe
The word superfood is thrown around fairly easily nowadays. Sometimes, it's an accurate description of highly nutritious foods that carry potent health-boosting properties. Other times it's a clever marketing ploy,...
Low Histamine Broccoli Bread Recipe
The word superfood is thrown around fairly easily nowadays. Sometimes, it's an accurate description of highly nutritious foods that carry potent health-boosting properties. Other times it's a clever marketing ploy,...

Low Histamine Coconut and Kale Fried Rice Recipe
Fried rice can be a wholesome, hearty meal that fills you up and keeps you feeling satisfied when you're craving some carbs. But, with all of that soy sauce, lemon...
Low Histamine Coconut and Kale Fried Rice Recipe
Fried rice can be a wholesome, hearty meal that fills you up and keeps you feeling satisfied when you're craving some carbs. But, with all of that soy sauce, lemon...

How Hormones Impact Histamine Intolerance
Did you know that women are more likely to be histamine intolerant? Well, today we're going to get into the fascinating link between the role that hormones play in those born...
How Hormones Impact Histamine Intolerance
Did you know that women are more likely to be histamine intolerant? Well, today we're going to get into the fascinating link between the role that hormones play in those born...

Histamine Intolerance FAQ with Anita Tee
Today I'd like to share a bit more about my personal story of how I solved my histamine intolerance. I have dealt with so many clients over the years,...
Histamine Intolerance FAQ with Anita Tee
Today I'd like to share a bit more about my personal story of how I solved my histamine intolerance. I have dealt with so many clients over the years,...

Salicylate Intolerance and Histamine Symptoms
So you're eating low histamine, but still reacting! Now what? Are you meticulously following a low histamine diet? Have you taken into account other histamine contributors such as hormones, stress...
Salicylate Intolerance and Histamine Symptoms
So you're eating low histamine, but still reacting! Now what? Are you meticulously following a low histamine diet? Have you taken into account other histamine contributors such as hormones, stress...

Is Histamine Intolerance Genetic? DAO, HNMT, MT...
Your genes dictate who you are, and this is true for what happens both from a physical and a biological perspective!Think about your eye and hair color. You weren’t randomly...
Is Histamine Intolerance Genetic? DAO, HNMT, MT...
Your genes dictate who you are, and this is true for what happens both from a physical and a biological perspective!Think about your eye and hair color. You weren’t randomly...

Low Histamine Faux Banana Bread Recipe
It’s a distinct smell. Not too sweet, but just sweet enough. It brings back childhood memories of warm, soft, butter-laden treats… oh, to be able to eat a glorious slice...
Low Histamine Faux Banana Bread Recipe
It’s a distinct smell. Not too sweet, but just sweet enough. It brings back childhood memories of warm, soft, butter-laden treats… oh, to be able to eat a glorious slice...

Low Oxalate Diet: How it Can Help Your Histamin...
Are you struggling to manage your histamine symptoms? Well... have you ever heard about oxalates? Are you histamine intolerant and have previously or currently: had a problem with candida...
Low Oxalate Diet: How it Can Help Your Histamin...
Are you struggling to manage your histamine symptoms? Well... have you ever heard about oxalates? Are you histamine intolerant and have previously or currently: had a problem with candida...

Histamine Intolerance Genetics and Gene Mutations
Did your histamine intolerance start in your genes?Constant headaches that often turn into migraines. Anxiety, irritability and mood disturbances. Nausea, digestive symptoms and reactions to even healthy foods. Constant runny...
Histamine Intolerance Genetics and Gene Mutations
Did your histamine intolerance start in your genes?Constant headaches that often turn into migraines. Anxiety, irritability and mood disturbances. Nausea, digestive symptoms and reactions to even healthy foods. Constant runny...

What Causes Histamine Intolerance? 4 Common Causes
If you’ve been suffering from histamine intolerance, and reacting to foods with outbreaks of symptoms such as hives, skin rashes and digestive symptoms, you’re probably wondering how you got here...
What Causes Histamine Intolerance? 4 Common Causes
If you’ve been suffering from histamine intolerance, and reacting to foods with outbreaks of symptoms such as hives, skin rashes and digestive symptoms, you’re probably wondering how you got here...

How to Approach Histamine Intolerance with your...
Living with a histamine intolerance can be maddening. Not just frustrating… maddening.What, with the long list of symptoms you can't quite pinpoint to anything specific you ate or did, plus the brushing off...
How to Approach Histamine Intolerance with your...
Living with a histamine intolerance can be maddening. Not just frustrating… maddening.What, with the long list of symptoms you can't quite pinpoint to anything specific you ate or did, plus the brushing off...

Gut Health, Leaky Gut and Histamine Intolerance
Do you have a high level of suspicion that you’re histamine intolerant?Well, if your body just doesn’t seem to be coping with the amount of this compound, and it’s leaving...
Gut Health, Leaky Gut and Histamine Intolerance
Do you have a high level of suspicion that you’re histamine intolerant?Well, if your body just doesn’t seem to be coping with the amount of this compound, and it’s leaving...

Low Histamine Baked French Toast Recipe
You have invited your family over for brunch. And you really want to spoil them. But... you don’t want to end up feeling miserable on the sofa in the afternoon...
Low Histamine Baked French Toast Recipe
You have invited your family over for brunch. And you really want to spoil them. But... you don’t want to end up feeling miserable on the sofa in the afternoon...

Migraine Headaches and Histamine Intolerance
Migraine: if you suffer with these intense headaches, all I need to do is mention the word to put you in defensive mode. They often even let you know...
Migraine Headaches and Histamine Intolerance
Migraine: if you suffer with these intense headaches, all I need to do is mention the word to put you in defensive mode. They often even let you know...

Antihistamine Maple Ginger Chicken Recipe
Who doesn’t love a low histamine chicken dinner? Or, better yet, an anti-histamine chicken dinner! These chicken thighs are a taste sensation for the whole family to enjoy. Everyone will love them...
Antihistamine Maple Ginger Chicken Recipe
Who doesn’t love a low histamine chicken dinner? Or, better yet, an anti-histamine chicken dinner! These chicken thighs are a taste sensation for the whole family to enjoy. Everyone will love them...

Is Histamine Intolerance Real?
How many times have you visited your doctor for advice and treatment for seemingly random symptoms? It could be gastrointestinal issues like IBS, bloating or constipation. Maybe your skin...
Is Histamine Intolerance Real?
How many times have you visited your doctor for advice and treatment for seemingly random symptoms? It could be gastrointestinal issues like IBS, bloating or constipation. Maybe your skin...

The Link Between Gluten and Histamine Intolernace
Have you been having tummy troubles? Do you struggle with constipation or diarrhea, pain and/or bloating?What about your mood - are you feeling depressed or anxious? A lot of these...
The Link Between Gluten and Histamine Intolernace
Have you been having tummy troubles? Do you struggle with constipation or diarrhea, pain and/or bloating?What about your mood - are you feeling depressed or anxious? A lot of these...

Pain Medication and Histamine Intolerance Symptoms
Could your pain medication be contributing to your histamine symptoms? Let's find out...We all use them here and there. Many of them we can buy over the counter. They offer...
Pain Medication and Histamine Intolerance Symptoms
Could your pain medication be contributing to your histamine symptoms? Let's find out...We all use them here and there. Many of them we can buy over the counter. They offer...

Turmeric and Histamine Intolerance Symptoms
Have you heard much about the impact of turmeric on histamine intolerance symptoms? Turmeric is an orange spice commonly used in curries and other flavorful. But did you know that it...
Turmeric and Histamine Intolerance Symptoms
Have you heard much about the impact of turmeric on histamine intolerance symptoms? Turmeric is an orange spice commonly used in curries and other flavorful. But did you know that it...


