
Klebsiella and Histamine Intolerance
Klebsi-who? And it lives in my digestive system?You’ve gone through the trouble of getting a stool test done to get a little bit closer to the answer you’ve been seeking: what’s happening...
Klebsiella and Histamine Intolerance
Klebsi-who? And it lives in my digestive system?You’ve gone through the trouble of getting a stool test done to get a little bit closer to the answer you’ve been seeking: what’s happening...

Histamine Intolerance, Estrogen and Hormonal Im...
Your hormones are there to tightly regulate many critical processes that take place in your body. When they’re doing their job, you have loads of energy, you’re fit and strong,...
Histamine Intolerance, Estrogen and Hormonal Im...
Your hormones are there to tightly regulate many critical processes that take place in your body. When they’re doing their job, you have loads of energy, you’re fit and strong,...

Eosinophilic Esophagitis and Histamine Intolerance
Did you know that eosinophilic esophagitis is another underlying cause of histamine intolerance to consider?... let's dive in. Histamines? Check… You’re well aware of what they do, where they come...
Eosinophilic Esophagitis and Histamine Intolerance
Did you know that eosinophilic esophagitis is another underlying cause of histamine intolerance to consider?... let's dive in. Histamines? Check… You’re well aware of what they do, where they come...

Histamine Intolerance in Children and Babies
Feeding toddlers can be a challenging task. Between dealing with their varying appetite, short attention span and picky eating habits, a parent has their work cut out for them.This task...
Histamine Intolerance in Children and Babies
Feeding toddlers can be a challenging task. Between dealing with their varying appetite, short attention span and picky eating habits, a parent has their work cut out for them.This task...
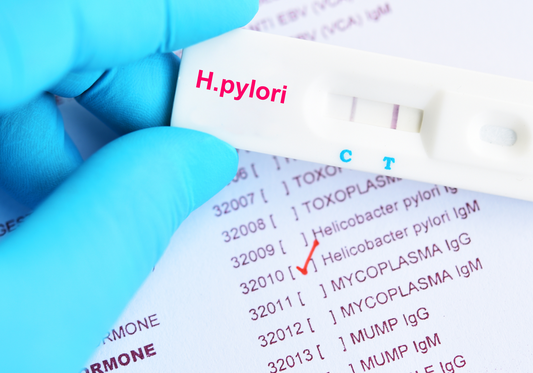
H. pylori and Histamine Intolerance: Top 7 Natu...
Most histamine intolerant individuals are working to rebalance their gut bacteria using histamine safe probiotics. This is because bacterial issues and histamine intolerance tend to go hand-in-hand. But, did you know...
H. pylori and Histamine Intolerance: Top 7 Natu...
Most histamine intolerant individuals are working to rebalance their gut bacteria using histamine safe probiotics. This is because bacterial issues and histamine intolerance tend to go hand-in-hand. But, did you know...

Low Histamine "No-Oatmeal" Recipe
While oatmeal is part of the low histamine food list, some people just don’t tolerate grains while their digestive system is in distress, and so, even if you are craving...
Low Histamine "No-Oatmeal" Recipe
While oatmeal is part of the low histamine food list, some people just don’t tolerate grains while their digestive system is in distress, and so, even if you are craving...

Heat Intolerance, Cold Intolerance & Histamine
If you're often feeling too hot or too cold, and have an issue regulating your temperature, perhaps histamine is to blame... When everyone is telling you that being outside in...
Heat Intolerance, Cold Intolerance & Histamine
If you're often feeling too hot or too cold, and have an issue regulating your temperature, perhaps histamine is to blame... When everyone is telling you that being outside in...

How to Get a Histamine Intolerance Diagnosis
It is common for someone with histamine intolerance to struggle for years to find answers to their problems. It can seem like every part of your body is affected. You...
How to Get a Histamine Intolerance Diagnosis
It is common for someone with histamine intolerance to struggle for years to find answers to their problems. It can seem like every part of your body is affected. You...

Histamine Intolerance Frequently Asked Questions
I always get plenty of questions about histamine intolerance. From diet to supplements to what the heck can be done to fix the condition, and everything in between, it seems...
Histamine Intolerance Frequently Asked Questions
I always get plenty of questions about histamine intolerance. From diet to supplements to what the heck can be done to fix the condition, and everything in between, it seems...

Low Histamine Warm Broccoli Salad Recipe
Do you sometimes avoid salads because of histamine intolerance? It’s no secret: despite being super healthy, those of you with histamine intolerance typically stay far, far away from salads. Not...
Low Histamine Warm Broccoli Salad Recipe
Do you sometimes avoid salads because of histamine intolerance? It’s no secret: despite being super healthy, those of you with histamine intolerance typically stay far, far away from salads. Not...

I'm Eating Healthy. So Why Do I Have Histamine ...
Do you ever wonder the role eating has played in the development of your histamine intolerance?For example, when you noticed you didn’t feel as well as you used to, and...
I'm Eating Healthy. So Why Do I Have Histamine ...
Do you ever wonder the role eating has played in the development of your histamine intolerance?For example, when you noticed you didn’t feel as well as you used to, and...

Common Food Additives and Histamine Intolerance
Have you ever questioned whether you might have a food intolerance? All those little - and sometimes not so little - signs and symptoms must mean something. The chronic...
Common Food Additives and Histamine Intolerance
Have you ever questioned whether you might have a food intolerance? All those little - and sometimes not so little - signs and symptoms must mean something. The chronic...

Low Histamine Chicken Stir Fry and Sauce Recipe
I love a good stir fry recipe - it's a super easy way to get in loads of nutritious, natural foods while still feeling like a delicious treat. Of course,...
Low Histamine Chicken Stir Fry and Sauce Recipe
I love a good stir fry recipe - it's a super easy way to get in loads of nutritious, natural foods while still feeling like a delicious treat. Of course,...

Bloating and Histamine Intolerance
There are few things that are worse than bloating. A swollen and full belly not only feels really uncomfortable, it can really ruin your day.You feel like your clothes don’t...
Bloating and Histamine Intolerance
There are few things that are worse than bloating. A swollen and full belly not only feels really uncomfortable, it can really ruin your day.You feel like your clothes don’t...
Histamine Intolerance and Your Liver
Are you living with histamine intolerance? Well today, you're going to find out why it's important to pay attention to and take care of your liver when suffering from histamine...
Histamine Intolerance and Your Liver
Are you living with histamine intolerance? Well today, you're going to find out why it's important to pay attention to and take care of your liver when suffering from histamine...

Is Exercise Causing Your Histamine Intolerance ...
Have you ever wondered if there's a link between exercise and histamine intolerance?Whether exercise can reduce histamine levels? Or whether your symptoms get worse through exercise induced histamine release?You may have...
Is Exercise Causing Your Histamine Intolerance ...
Have you ever wondered if there's a link between exercise and histamine intolerance?Whether exercise can reduce histamine levels? Or whether your symptoms get worse through exercise induced histamine release?You may have...

Low Histamine Pulled Chicken Spaghetti Squash R...
I've dealt with many clients who are just at their wits end with histamine intolerance. They’re frustrated with their bland food and the symptoms they experience when they deviate...
Low Histamine Pulled Chicken Spaghetti Squash R...
I've dealt with many clients who are just at their wits end with histamine intolerance. They’re frustrated with their bland food and the symptoms they experience when they deviate...

Superfood Low Histamine Smoothie Recipe
Are you looking for a low histamine smoothie to kickstart your breakfast routineHaving trouble packing in those morning greens?If you’re histamine intolerant and aiming for a vibrant burst of breakfast nutrients,...
Superfood Low Histamine Smoothie Recipe
Are you looking for a low histamine smoothie to kickstart your breakfast routineHaving trouble packing in those morning greens?If you’re histamine intolerant and aiming for a vibrant burst of breakfast nutrients,...

Roasted Low Histamine Salad Recipe
Ready for a warm twist on the typical raw low histamine saladWell, you're in luck because it's salad time!Nothing beats a salad when it comes to a super easy way...
Roasted Low Histamine Salad Recipe
Ready for a warm twist on the typical raw low histamine saladWell, you're in luck because it's salad time!Nothing beats a salad when it comes to a super easy way...

Low Histamine Beet and Berry Smoothie Recipe
What part of the body do you eat with?If you said your mouth, you’re not wrong… technically. The truth is, we mostly ‘eat’ with our eyes first!Think about it, you...
Low Histamine Beet and Berry Smoothie Recipe
What part of the body do you eat with?If you said your mouth, you’re not wrong… technically. The truth is, we mostly ‘eat’ with our eyes first!Think about it, you...

How to Block Nighttime Histamine Release
You’re fast asleep. You're not eating, you're not drinking and you haven’t taken any medication for hours. And yet, you wake up in the early hours of the morning with...
How to Block Nighttime Histamine Release
You’re fast asleep. You're not eating, you're not drinking and you haven’t taken any medication for hours. And yet, you wake up in the early hours of the morning with...

Why Food Triggers Histamine Symptoms
You’ve seen a list. Maybe you’ve seen many different lists…Lists that tell you which foods you should be avoiding because of the histamine flare ups you're getting, in the hope...
Why Food Triggers Histamine Symptoms
You’ve seen a list. Maybe you’ve seen many different lists…Lists that tell you which foods you should be avoiding because of the histamine flare ups you're getting, in the hope...

How GMO’s and Glyphosate Impact Histamine Intol...
There’s no question that food can affect your tolerance to histamine.There is, however, a question about what exactly is in the food you eat that leads to a poorer tolerance...
How GMO’s and Glyphosate Impact Histamine Intol...
There’s no question that food can affect your tolerance to histamine.There is, however, a question about what exactly is in the food you eat that leads to a poorer tolerance...

Low Histamine Smoothie Bowl AND Granola Recipe!
Oh boy have I got a treat for you... a low histamine smoothie bowl recipe that's even complete with granola!Did you ever think you’d be able to eat granola again?...
Low Histamine Smoothie Bowl AND Granola Recipe!
Oh boy have I got a treat for you... a low histamine smoothie bowl recipe that's even complete with granola!Did you ever think you’d be able to eat granola again?...


