If you've been itching and scratching in response to food, developing hives and anxiety and even digestive issues to boot, there's a chance you may have histamine intolerance.
What’s histamine intolerance, you ask? Well, it’s a very under-recognized disorder that may be behind all of your strange, allergy-like symptoms.
And why is it under-recognized? Because conventional medical practitioners will usually chalk your symptoms up to everything but a histamine intolerance. Your runny, itchy nose? It's seasonal allergies, they'll say. Your digestive issues? Oh, surely that's because of your diet! And your headaches? Those are because you're stressed, your neck is tense, and you don't have good posture...
What we know, however, is that they can all be linked, and all because your body is not coping with the amount of histamine it contains.
That's why today, I want to give you the lowdown on everything you need to know about histamine intolerance so that you can help to facilitate the best approach to your treatment and, best of all, address the cause of your symptoms so that you're not only able to manage them, but overcome them altogether.
Let's get started...
What Exactly Is Histamine Intolerance?
When you consider a typical food allergy, the reaction the body produces as a result of coming into contact with that food compound causes the immune system to produce severe and rapid symptoms. Coming into contact with the food can cause anaphylaxis, which can potentially be fatal.
A histamine intolerance is not an allergy to histamine; instead, it's an intolerance to the compound due to a problem that develops when your body is unable to cope with the amount of histamine in your system. Now, as you'll read more about below, because histamine is a necessary compound that's part of the immune system, it has far-reaching effects on the body, acting in every tissue and organ. It's for this reason that histamine intolerance can be the cause of such body-wide reactions and produce seemingly unrelated symptoms.
To understand how and why histamine can cause a problem, let’s begin to explore the reasons behind this intolerance by answering a few questions…
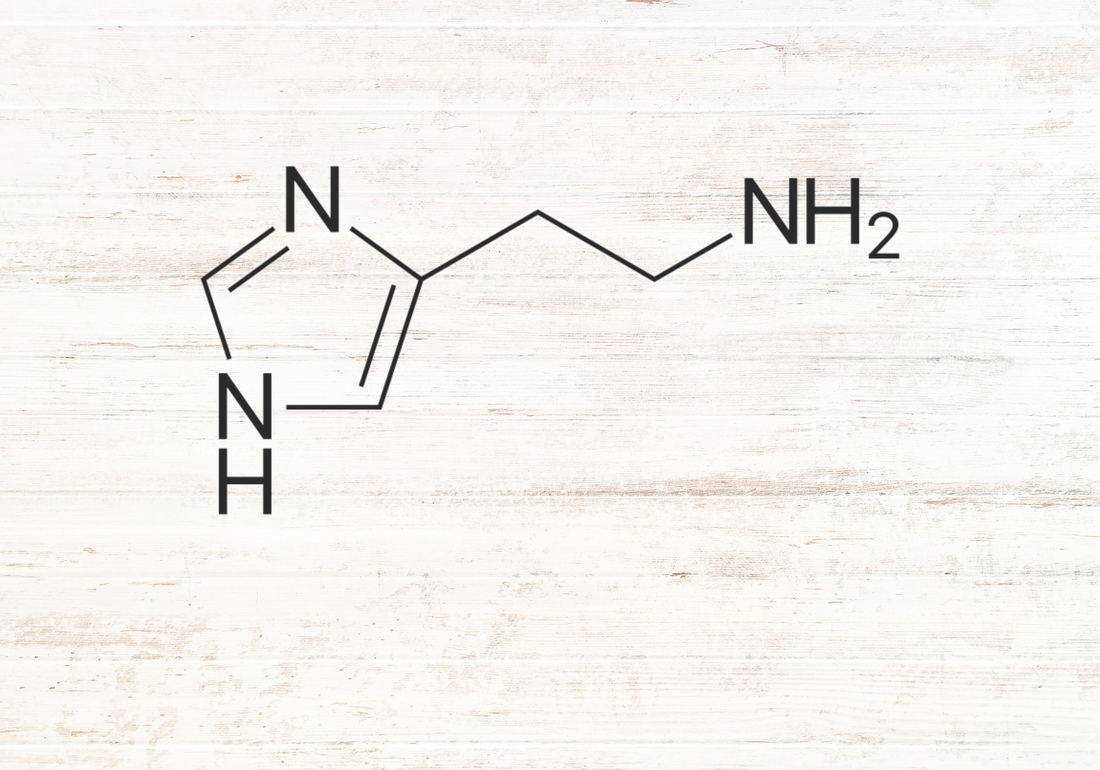
1. What is histamine?
While histamine is a chemical messenger compound that acts as a signal to communicate between the immune system and various cells. It is also involved in processes like stomach acid secretion, which is involved in digestion, your sleep-wake cycles (1), and even brain function, or cognition (2). The main action of histamine, however, that we’re interested in today, is its role in the immune system.
Histamine is a compound the body makes in various cells located across all of the body's tissues, which is part of the defense pathway when the local immune system is triggered. The compound acts to neutralize any substance the body views as a threat, and it is produced and contained in different types of cells, of which mast cells and basophils are most noteworthy when it comes to the immune system (3).
Mast cells are located in high concentrations in the skin, lungs, nose, mouth, digestive tract and the bloodstream (4), while basophils are a type of white blood cell that are brought to the site where they are needed only to attack a foreign invader once the immune response has been triggered (5).
2. What causes the body to release histamine?
There are a number of reasons for histamine release to occur, but it is typically as a result of the immune system feeling unsafe, or under threat. Cells that are part of the immune system pick up foreign proteins in the blood, and trigger a cascade of actions to help to neutralize them. Because proteins are the building blocks of many functions in the body, these foreign proteins could cause havoc to the way the body works, and so it's important to neutralize them as soon as possible.
When you’re stung by a bee, for example, the body recognizes the protein within the venom as a threat and histamine jumps into action to immediately bring help to the site where the venom has been injected. Swelling, itching and redness occur as a result of histamine's actions.
Now, this is an action of histamine that has some real value. The venom may cause serious damage to the body's tissue. Sometimes, the immune system gets it wrong, and reacts even if the substance that comes into contact with the body is not necessarily harmful. But because the immune system still perceives it as a threat, histamine goes to work.
This is what happens when the immune system sees substances such as pollen, dust, pet dander, chemicals, and even foods in your daily diet as a threat, and triggers the release of histamine (6). It's these everyday reactions that can cause histamine levels in the body to rise above those expected, which can lead to histamine intolerance.
3. What does histamine do?
When released by the mast cells, histamine triggers other systems of the body to jump into action. Throughout the body, there are locations on specific cells, called receptors, which allow histamine to bind in a lock-and-key fashion. Once histamine locks into these receptors, it switches on a response. The four known histamine receptors are denoted H1, H2, H3 and H4 and, depending on their location, a specific response is elicited (7).
H1: They are expressed on the cells that line certain organs like the nose, mouth and digestive system. They are also located within the muscle tissue of the lungs, which is a major source of allergic reaction due to inhaled triggers (8). Within the brain and spinal cord, H1 receptor activation triggers behavioral effects and excitement, which contributes to the feeling of being hyper alert.
H2: Located within the stomach, these receptors turn on the processes involved in the stomach releasing stomach acid (9).
H3: Within the brain and spinal cord, H3 receptor activation plays a role in behavioral effects as well as body temperature changes (10).
H4: The most recently discovered histamine receptor is one involved in the regulation of all other immune system cells, and plays a role in activating or inhibiting their functions (11,12).
When histamine binds to any of these receptors, some system in the body is activated. For example, when histamine binds to the H1 or H2 receptors located in the heart muscle (13), it causes the heart to beat faster to ensure that blood can pump through the body at an increased pace in order to bring other nutrients and working cells to the site of the threat more quickly. At the same time, different types of histamine receptors across the body may be activated, depending on where the histamine is being concentrated.
The more histamine is released, the more these receptors are activated, the higher the response will be felt throughout the body. When histamine release is triggered in an ongoing fashion, for example when you're constantly being exposed to pollen, dust or dander, it leaves you with a multitude of chronic undesirable symptoms.
Chronic histamine release and/or a reduced capacity of the body to manage and get rid of it results in internal histamine levels being too high. When levels are too high, it causes chronic reactions with even the slightest histamine increase. This is the condition we know as histamine intolerance (14).
With even slight increases in histamine - whether they're in response to a real threat or not - it will typically cause a slew of bothersome symptoms. These symptoms are typically widespread throughout the body and, thinking back to where the histamine receptors are located in tissues expanding across the span of the body, it explains why a reaction can affect every system and cause it to malfunction.
So, what is it that causes high histamine levels, and how can you help the body to manage histamine levels like it should?
Four Main Factors That Cause High Histamine Levels
There are several causes of histamine intolerance. Below are four of the main ones that could be impacting your body.
1. Enzyme insufficiency
Your body has two primary ways of breaking down histamine. Both involve enzymes, where one is called diamine oxidase (DAO) and the other, histamine N-methyltransferase (HNMT). If these enzymes are in short supply, histamine levels rise and are not appropriately lowered back down to normal level.
DAO is a more widespread means of histamine breakdown, whereas HNMT breaks down histamine within cells (15).
Problems with DAO can either be as a result of it being made in short supply, or as a result of it being used up in other processes leaving too little available for the breakdown of histamine. Certain medications like non-steroidal anti-inflammatory drugs (NSAIDs) may also block the formation and release of DAO while simultaneously increasing the release of histamine. Certain foods, which you will learn more about in the sections below, may have the same effects.
One of the fastest and most effective therapies for this issue is to simply use an all-natural DAO enzyme supplement. Supplementing this enzyme can replenish low levels, therefore helping to break down histamine in the body and improve associated symptoms.
2. Bacterial overgrowth
Because some of the bacteria that live in your gut release histamine, too many of these certain types can elevate the levels of histamine your body has to deal with. Fungus that can overgrow in the gut - like candida, for example - promotes histamine release as a way the body tries to deal with the overgrowth and kill off the excess fungus.
It's not just bothersome bacteria that are a problem. Believe it or not, even ‘good’ bacteria convert the amino acid histidine into histamine - a usually harmless process.
The bacterial contribution to histamine intolerance is a really important consideration. If you take just any probiotic you'll typically buy off the shelf - even helpful ones - it can actually make histamine intolerance symptoms worse!
Fortunately, I have a great probiotic formula targeted for those with histamine intolerance. You can also find a list of low histamine probiotics that are safe for histamine intolerance as well as high histamine probiotics to stop taking immediately in this blog article.
3. Mast cells
Histamine is typically released from mast cells in response to allergens, however, if mast cells are unstable or become overactive, histamine can be released at higher-than-normal levels.
Mast cell destabilization and malfunction can occur for many reasons, such as an H. pylori infection or other biological or inherited dysfunctions.
Most histamine intolerance sufferers will experience mast cell issues to at least some degree, and it’s why the most common and effective therapy I use is a particularly potent mast cell stabilizer, which has allowed the majority of my clients to eat more foods with less symptoms, in as little as 10 days. You can find my recommendation for the top histamine supplement here.
4. Digestive disorders
The term leaky gut is commonly used to describe the cause of a range of different health issues. But what is it?
Well, normally, the digestive tract is selectively permeable, meaning it allows certain nutrients to pass through the gut and enter the body while also filtering out potential threats such as toxic compounds, pathogens and whole food particles.
This mechanism allows us to let the good stuff in, while keeping the bad stuff out. Make sense?
When leaky gut has developed, on the other hand, the digestive tract has become even more permeable, meaning larger molecules are allowed to move into the bloodstream, which would normally be filtered out and eliminated from the body.
When these larger molecules enter the bloodstream, the body does not recognize them and therefore reacts with an immune response, involving inflammation and histamine release.
Not only does this scenario place more demand on the DAO enzyme to reduce histamine levels, but inflammation in the gut decreases DAOs ability to perform and further contributes to the problem.
While there are far more causes of histamine intolerance, these are the main four I usually come across with my clients. As a result of any of these or a combination of them, it'll cause you to experience the symptoms of chronically high histamine levels.
Getting to Know the Symptoms of Histamine Intolerance
High histamine levels result in a variety of symptoms, often corresponding to the receptors that histamine normally binds to and activates. We can, therefore, categorize the symptoms into the areas of the body where these histamine receptors are found:
Nervous system symptoms:
The most common symptom of histamine intolerance that affects the nervous system is headaches. In fact, for those of you that suffer with migraines, it's commonly as a result of high histamine levels.
Research agrees! Evidence suggests that headaches or migraines arising from the consumption of alcohol may be more likely to develop due to histamine reactions rather than from the alcohol itself (16).
Lung and respiratory tract symptoms:
Respiratory manifestations as a result of high histamine levels include runny nose, wheezing, difficulty breathing, coughing and asthma-like symptoms (17).
Skin symptoms:
Atopic dermatitis and chronic urticaria are associated with histamine intolerance, as are flushing, swelling, itching and increased warmth in the skin upon acute increase in the body’s histamine levels (18).
Reproductive system symptoms:
Women who have histamine intolerance may have associated irregularities in their menstrual cycle and suffer more frequent headaches during menstruation due to the link between histamine and female sex hormones that correlate with reproduction (19).
Digestive Symptoms:
The digestive tract not only has a high concentration of histamine receptors, the bacteria that live in your gut also produce histamine during their role in food breakdown and, when you add the foods you consume that are higher in histamine, there’s little wonder why histamine intolerance results in such severe digestive disturbances like cramps, diarrhea, flatulence and bloating (20).
High histamine levels have also been implicated in a number of digestive diseases like Crohn’s, ulcerative colitis, food allergies and even colorectal cancer (21).
It is the role of histamine in the early response of inflammation that causes these symptoms, which may be either acute/short-acting, or chronic/long-standing (22).
I’ve created a blog post which contains a more comprehensive list of histamine intolerance symptoms, so be sure to check it out!
Now, you may be looking at the symptoms in the body systems above and asking the question: how do you know if you have histamine intolerance? To obtain an answer, think about when your symptoms are most severe.
- Do you get a runny nose and itchy eyes after you eat tomatoes, avocados or drink tea?
- Do you have a diagnosed food allergy or intolerance?
- Do you often suffer from sinusitis, asthma-like symptoms or experience flushing of the face and neck when you drink even small amounts of alcohol?
Any of these can indicate that your body is just not coping with its histamine levels, and you need to do something about it to find relief. Fortunately, there are a few ways you can help your body out. And, one of the quickest ways to improve symptoms and confirm your histamine intolerance is to address your diet...
Here’s How to Discover Which Foods Are Causing Your Histamine Intolerance
To start giving your body the break it needs, you need to look at the foods that are high in histamine, so that you may begin to reduce them in the diet.
How does diet play a role? Well, because of how histamine activation works in the gut.
The foods on the following list influence histamine in a number of ways. They can either:
- Increase the amount of histamine released into the body (these are histamine-releasing foods)
- Block that enzyme we mentioned earlier, called DAO and the enzyme responsible for degrading histamine (these are DAO-blocking foods); or
- They are simply higher in histamine levels, which increases the amount the body has to deal with (high histamine foods)
Below is a general list of foods and medications that impact histamine intolerance. This list is not fully comprehensive, but I've created a post with a comprehensive list of high and low hismine foods.
For a quick overview, let’s start with the foods that are high in histamine that you need to stay away from as much as you can:
- Coffee
- Dates
- Black and green tea
- Avocado
- Mushroom
- Spinach
- Green bell peppers
- Legumes (including green peas and red beans)
- Processed and aged meat (salami, sausage, etc)
- Tomatoes
- Banana
- Vinegar and pickled items
- Commercial salad dressings with vinegar
- Raw egg
- Preservatives
- Cheese (all processed and fermented varieties)
- Soy and soy products
- Kefir and yogurt
- Milk
- Shellfish
- Tartrazine
- Citrus fruit (this includes oranges, lemons and limes)
- Strawberries
- Pineapple
- Pumpkin
- Dried fruit
- Walnuts and cashews
- Over-ripe vegetables
- Any leftover food not stored in the fridge immediately after cooking
- Chocolate and cocoa
- Alcohol
- Fermented cabbage
- Yeast containing breads and cakes
- Sourdough
- Sour cream
- Eggplant
- Pineapple (bromelain, the pineapple extract however, can actually act as a natural antihistamine)
- Olives (not their oils)
- Mayonnaise
But WAIT! Before you shout out in protest and demand to know what you can eat... believe it or not, the list is actually longer. Here’s a list of low-histamine foods you can still enjoy:
- Sweet potato
- Melon
- Red lettuce
- Cucumber
- Rice (brown/wild/red jasmine/black)
- Fresh corn
- Zucchini
- Red apple
- Blueberries
- Cauliflower
- Grapes
- Peach
- Carrots
- Leek
- Radish
- Broccoli
- Beetroot (fresh)
- Chinese cabbage
- Egg (completely cooked)
- Fennel
- Apricot
- Artichoke
- Pomegranate
- Litchi
- Mango
- Butternut squash
- Milk substitutes (rice, hemp, oat)
- Leafy herbs like basil, thyme, rosemary, sage, oregano, peppermint
- Gluten-free wholegrains like quinoa, millet, sorghum, buckwheat
- Fresh beans and lentils (not red)
- Coconut milk
- Red onions
- Raw honey
- Chia seeds
- Hemp seeds
- Sesame, sunflower, pumpkin (pepita) seeds
- Garlic
- Red cabbage
- Asparagus
- Olive and coconut oil
- Pure peanut butter (natural, without any other ingredients added)
- Turmeric
- Ginger
- Flaxseed meal
- Cantaloupe
- Freshly caught and gutted fish
- Freshly cooked meat and poultry
- Any other vegetable not mentioned on the foods to reduce list
- Herbal tea
By controlling histamine levels with your diet, you can control how much external histamine you’re putting into your body, and in doing so, reduce the load your body has to deal with (23,24).
Other Common Sources of Histamine Affecting the Body
On top of foods, there are also drugs or medications that may increase histamine release, promote its liberation, or block the DAO enzyme. These include some specific types of (23):
- Antidepressants
- Muscle relaxants
- Pain relievers
- Anaesthetics
- Blood pressure medication
- Antiarrhythmics
- Diuretics
- Antibiotics
- Anti-hypnotics
- Mucolytics
- H2 receptor blockers
If you are on one of these classes of medication and you continue to suffer from histamine intolerance, speak to your doctor about your alternative options when it comes to their histamine influence.
If you manage the external factors like food and medication, it provides a simple and immediately effective method on how to reduce histamine release from your body.
Now that you know what histamine intolerance is, how you develop it and the diet you can follow to reduce its effects, let’s get into how histamine intolerance is treated.
Wondering How Histamine Intolerance Is Treated? Here’s Some Help!
Unfortunately, histamine intolerance is one of those difficult to diagnose conditions as the symptoms are so vast, and they affect many different organ systems.
Individuals may have a range of different symptoms and so a diagnosis is typically based on a thorough history taking, and a look into the trigger of the symptoms. One of the best ways the body will indicate that there’s an issue with histamine load is through the development of symptoms (24) after eating or drinking high histamine foods. The best way to achieve a diagnosis is through the help of a healthcare professional, such as a doctor knowledgeable in functional or integrative medicine, a naturopath, or a qualified nutritional therapist.
Should these professionals not be an option for you to approach right now, there’s a process you can follow yourself to determine if histamine may be a problem for you:
Step 1: Log your symptoms
Start taking note of the symptoms mentioned above when these foods are still in your diet. Continue to monitor your symptoms for 5 days to a week. Note that symptoms may not come on immediately; they can develop over the course of a couple of days. On your food and drinks log, highlight the high histamine foods and look to correlate the symptoms you experience in the time frame following their ingestion.
Step 2: Go low histamine
Now, for the next 10-14 days, dramatically reduce your intake of high histamine foods on the ‘avoid’ list, and only consume ‘allowed’ foods according to this low histamine diet food list. Continue to take note of your symptoms during this time.
It’s important to be quite strict in this phase in order to make the most of your body’s ability to reduce the current histamine load.
Step 3: Reintroduce and track
Lastly, reintroduce one or two higher histamine foods at a time and take note of your symptoms. This phase may last up to 6 weeks. Also take note as to whether there are external influencing factors at play, like stress, the use of medication, or menstruation, for example (25).
If you develop symptoms in response to the high histamine food reintroduction, this is a strong indication that histamine is not being effectively broken down by your body. It’s likely time to start a histamine intolerance protocol to help you to determine why, and what your next steps can be to start your journey to health and wellbeing.
For a more comprehensive at-home test for histamine intolerance, read my blog post about it here.
Looking for Testing Options for Histamine Intolerance? This Might Be the Best Approach…
Although tests for histamine intolerance have been proposed in various scientific studies, the majority have limited availability or are not available for public use.
Most reliable tests for histamine intolerance must be obtained through a specialized practitioner. Below is a breakdown of clinical methods for testing histamine intolerance:
1. Determining DAO activity in the blood or in the intestines
It may be valuable to determine how much DAO is active in the blood, however, there is evidence to suggest that this does not provide a conclusive result as DAO is active in a number of tissues when it is needed, instead of remaining in the bloodstream.
In the intestines, measurement of DAO activity may provide significant evidence as to whether there is a histamine issue; there is a need for more scientific evidence to be conducted regarding this testing method.
If DAO levels are found to be low, a fast and effective therapy can simply be to use an all natural DAO enzyme supplement.
2. Histamine 50-skin-prick test
While not available for public use, there has been development of a test that determines how quickly histamine is able to degrade in 50 minutes (30).
As this test measures how quickly your body breaks down histamine, it provides a great method for understanding if normal levels of histamine may cause a reaction due to a slower-than-normal degradation rate.
3. Stool tests for histamine intolerance
Because bacteria also produce histamine, it has been proposed that a stool analysis may give an indication as to what is going on with an individual’s histamine levels (27).
The very fact that these bacteria do produce histamine raises questions as to whether the amount of histamine in a stool sample is due to an increase in metabolism of it by the bacteria, or whether there is an intolerance or toxicity (28).
Here’s My Holistic Approach to Treating Histamine Intolerance
Mainstream medical treatment approaches to histamine intolerance symptoms typically involve the use of antihistamine pharmaceutical drugs or, in severe cases, steroids that suppress the immune system.
The most widely available antihistamines block H1 receptors, while there are also those available that target the H2 receptors in the gut. It has, however, been noted in a review study that these drugs only control the symptoms related to the histamine response and not the underlying cause of the disorder (29).
These drugs have also been proposed to work in an acute setting of histamine toxicity, which means they are not supposed to be taken long-term (30). If you’re looking to find out how to break down histamine naturally outside of the changes you can already start making to your diet, we can begin to explore supplementation.
How to Lower Histamine Naturally With Supplements
One of the areas of current research in histamine intolerance therapies involves the function, or rather dysfunction, of the DAO enzyme.
There have been implications that one of the most common causes of low DAO is genetics, which has resulted in an increase in the risk of histamine intolerance, or increased histamine sensitivity.
While there is plenty of evidence to support the fact that a low-histamine diet can reduce histamine levels within the body, a low histamine diet also improves DAO levels at the same time, allowing the body to really begin coping with the demand (31).
In addition to diet, another way to increase the activity of DAO is to increase the intake of the nutrients DAO needs to be produced and function.
1. Fatty acids. We already know the importance of fatty acids like omega 3s on our overall health. Now, we can add histamine intolerance to that list (32). A recent study has shown that long chain fatty acids, especially those of saturated and monounsaturated variety improve DAO activity. Olive oil, coconut milk, and coconut oil are good examples.
2. Low levels of copper, zinc and magnesium have also been implicated in reduced DAO activity. While there was no particular correlation between the increase in DAO and the intake of supplemental copper in experiments, DAO activity has been shown to increase with the addition of magnesium and zinc supplements (33).
3. DAO supplementation. In cases of low DAO enzymes, especially where genetics is the cause of low DAO production, a supplemental form of the enzyme may be necessary. In studies, DAO enzyme supplementation has shown to be effective in the treatment of histamine related symptoms, in particular episodes of headache or migraine in those with histamine intolerance (34,35).
4. Mast cell stabilizers. Histamine is released from mast cells within the body and, when histamine levels are too high, stabilizing mast cells can be a huge help for reducing the amount of histamine being released. The use of mast cell stabilizers therefore reduces the overall histamine levels in the body and calms symptoms, particularly when combined with DAO supplements (36,37). Natural mast cell stabilizers can act just like antihistamines in their ability to calm symptoms. The strongest natural mast cell stabilizer that I recommend to nearly all of my clients can be found here.
With more information and activity surrounding histamine intolerance in the media and online, scientists have started to pay attention. More studies are being conducted into the problem, and with it, comes more solutions. This change brings with it a significant amount of hope for all of us for the future of our condition.
Finally you have the evidence to support the fact that you are struggling with the daily chronic symptoms of histamine intolerance, having been told there’s nothing wrong, or that it’s just allergies.
With this Ultimate Guide to Histamine Intolerance in your toolkit, you can begin your plan of attack on histamine intolerance. Start making the changes to your diet and supplement routine right now to not only decrease your histamine levels but to enable your body to begin managing its histamine load on its own.
Now you can fight histamine intolerance and its long list of dreadful, debilitating symptoms… and win!
References:
- Thakkar MM. Histamine in the regulation of wakefulness. Sleep Med Rev. 2011;15(1):65-74. doi:10.1016/j.smrv.2010.06.004
- Provensi G, Costa A, Izquierdo I, Blandina P, Passani MB. Brain histamine modulates recognition memory: possible implications in major cognitive disorders. Br J Pharmacol. 2020;177(3):539-556. doi:10.1111/bph.14478
- Stone KD, Prussin C, Metcalfe DD (2010) IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol 125:S73–S80.
- Galli SJ, Tsai M (2012) IgE and mast cells in allergic disease. Nat Med 18:693–704.
- Karasuyama H, Mukai K, Obata K, Tsujimura Y, Wada T (2011) Nonredundant roles of basophils in immunity. Annu Rev Immunol 29:45–69.
- Yu, Y., Blokhuis, B. R., Garssen, J., & Redegeld, F. A. (2016). Non-IgE mediated mast cell activation. European Journal of Pharmacology, 778, 33–43.
- Borriello, F., Iannone, R., & Marone, G. (2017). Histamine Release from Mast Cells and Basophils. Histamine and Histamine Receptors in Health and Disease, 121–139.
- del Cuvillo A, Sastre J, Montoro J, Jáuregui I, Dávila I, Ferrer M, Bartra J, Mullol J, Valero A. Allergic conjunctivitis and H1 antihistamines. J Investig Allergol Clin Immunol. 2009; 19 Suppl 1():11-8.
- Hershcovici T, Fass R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol Sci. 2011 Apr; 32(4):258-64.
- Schwartz JC. The histamine H3 receptor: from discovery to clinical trials with pitolisant. Br J Pharmacol. 2011 Jun; 163(4):713-21.
- Reher TM, et al. Incomplete activation of human eosinophils via the histamine H4-receptor: evidence for ligand-specific receptor conformations. Biochem. Pharmacol. 2012;84:192–203.
- Liu WL (2014) Histamine H4 receptor antagonists for the treatment of inflammatory disorders. Drug Discov Today 19:1222–1225.
- Neumann J, Kirchhefer U, Dhein S, Hofmann B, Gergs U. The Roles of Cardiovascular H2-Histamine Receptors Under Normal and Pathophysiological Conditions. Front Pharmacol. 2021;12:732842. Published 2021 Dec 20. doi:10.3389/fphar.2021.732842
- Kovacova-Hanuskova, E., Buday, T., Gavliakova, S., & Plevkova, J. (2015). Histamine, histamine intoxication and intolerance. Allergologia et Immunopathologia, 43(5), 498–506.
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85:1185---96.
- Yuan, H., et al. Histamine and Migraine. The Journal of Headache and Pain. 2018. 58(1):184-193.
- Schnedl, W., & Queissner, R. Migraines appear more likely to be caused by histamine than ethanol. European Journal of Neurology. 2019.
- Hansen Selnø A.T., Sumbayev V.V., Raap U., Gibbs B.F. (2018) Role of Histamine in Inflammatory Diseases. In: Riccardi C., Levi-Schaffer F., Tiligada E. (eds) Immunopharmacology and Inflammation. Springer, Cham.
- Götz M., Jarisch R., Layritz C., Niederberger V., Raithel M. (2015) Disease Patterns in the Presence of Histamine Intolerance. In: Jarisch R. (eds) Histamine Intolerance. Springer, Berlin, Heidelberg.
- Maintz L, Schwarzer V, Bieber T, van der Ven K, NovakN. Effects of histamine and diamine oxidase activities on pregnancy: a critical review. Hum Reprod Update. 2008;14:485---95.
- Kovacova-Hanuskova, E., et al. Histamine, histamine intoxication and intolerance. Allergologia et immunopathologia. 2015.
- DeMeo, M., et al. Practical Gastroenterology and Hepatology Board Review Toolkit. John Wiley & Sons, 2016. 680 pages.
- Benly, P. Role of Histamine in Acute Inflammation. Pharm. Sci. & Res. Vol. 7(6), 2015, 373-376
- Prasad, K., et al. Histamine in Foods: Its Safety and Human Health Implications. J. Food Sci. Technol. Nepal, Vol. 8 (1-11 ) 2013.
- Vlieg-Boerstra BJ, van der HS, Oude Elberink JN, Kluin-Nelemans JC, Dubois AE. Mastocytosis and adverse reactions to biogenic amines and histamine-releasing foods: what is the evidence? Neth J Med 2005;63:244–9.
- Novotny WF, Chassande O, Baker M, Lazdunski M, Barbry P. Diamine oxidase is the amiloride-binding protein and is inhibited by amiloride analogues. J Biol Chem 1994;269:9921–5.
- Schnedl, W., et al. Evaluation of symptoms and symptom combinations in histamine intolerance. Intestinal Research 2019.
- Reese, I., Ballmer-Weber, B., Beyer, K. et al. German guideline for the management of adverse reactions to ingested histamine. Allergo J Int (2017) 26: 72.
- Yu, W., et al. Food allergy: immune mechanisms, diagnosis and immunotherapy. Nat Rev Immunol. 2016 Dec; 16(12): 751–765.
- Kofler L, Ulmer H, Kofler H. Histamine 50-skin-prick test: a tool to diagnose histamine intolerance. ISRN Allergy. 2011.
- Smolinska S, Jutel M, Crameri R, O’Mahony L. Histamine and gut mucosal immune regulation. Allergy. 2014;69:273–81.
- Miyoshi, M., Ueno, M., Matsuo, M., Hamada, Y., Takahashi, M., Yamamoto, M., … Usami, M. (2017). Effect of dietary fatty acid and micronutrient intake/energy ratio on serum diamine oxidase activity in healthy women. Nutrition, 39-40, 67–70.
- Kofler H, Aberer W, Deibl M, Hawranek TH, Klein G, Reider N, Fellner N. Diamine oxidase (DAO) serum activity: not a useful marker for diagnosis of histamine intolerance. Allergologie. 2009;32:105–9.
- Morrow JD, Margolies GR, Rowland J, Roberts LJ 2nd. Evidence that histamine is the causative toxin of scombroid-fish poisoning. N Engl J Med. 1991;324:716–20.
- Lackner, S., et al. Histamine-reduced diet and increase of serum diamine oxidase correlating to diet compliance in histamine intolerance. European Journal of Clinical Nutritionvolume 73, pages102–104 (2019).
- Izquierdo-Casas,J., et al. Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double-blind trial. Clinical Nutrition. 2019. 38(1):152-158.
- Schnedl, W.J., Schenk, M., Lackner, S. et al. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Sci Biotechnol (2019).

Anita Tee
My name is Anita Tee. I'm a nutritional scientist who specializes in histamine intolerance. I hold a Master of Science in Personalized Nutrition and a Bachelor of Science in Human Biology and Psychology.
For the past ten years, I have used my experience in nutritional and medical health sciences to create a scientifically backed, natural approach to healthcare that relies 100% on evidence-based research.
As I previously suffered from - and overcame - histamine intolerance, my focus is to increase recognition and expand the available resources and protocols available for resolving this particular disorder. To date, I have helped over 4,000 individuals fully resolve or better manage their histamine intolerance symptoms.